
U.S. Senate
See Full Big Line
(D) J. Hickenlooper*
(R) Somebody
80%
20%

Governor
See Full Big Line
(D) Joe Neguse
(D) Phil Weiser
(D) Jena Griswold
60%
60%
40%↓

Att. General
See Full Big Line
(D) M. Dougherty
(D) Alexis King
(D) Brian Mason
40%
40%
30%

Sec. of State
See Full Big Line
(D) George Stern
(D) A. Gonzalez
(R) Sheri Davis
40%
40%
30%

State Treasurer
See Full Big Line
(D) Brianna Titone
(R) Kevin Grantham
(D) Jerry DiTullio
60%
30%
20%

CO-01 (Denver)
See Full Big Line
(D) Diana DeGette*
(R) Somebody
90%
2%

CO-02 (Boulder-ish)
See Full Big Line
(D) Joe Neguse*
(R) Somebody
90%
2%

CO-03 (West & Southern CO)
See Full Big Line
(R) Jeff Hurd*
(D) Somebody
80%
40%

CO-04 (Northeast-ish Colorado)
See Full Big Line
(R) Lauren Boebert*
(D) Somebody
90%
10%

CO-05 (Colorado Springs)
See Full Big Line
(R) Jeff Crank*
(D) Somebody
80%
20%

CO-06 (Aurora)
See Full Big Line
(D) Jason Crow*
(R) Somebody
90%
10%

CO-07 (Jefferson County)
See Full Big Line
(D) B. Pettersen*
(R) Somebody
90%
10%

CO-08 (Northern Colo.)
See Full Big Line
(R) Gabe Evans*
(D) Yadira Caraveo
(D) Joe Salazar
50%
40%
40%

State Senate Majority
See Full Big Line
DEMOCRATS
REPUBLICANS
80%
20%

State House Majority
See Full Big Line
DEMOCRATS
REPUBLICANS
95%
5%
 February 21, 2024 10:39 AM UTC
February 21, 2024 10:39 AM UTC 3 Comments
3 Comments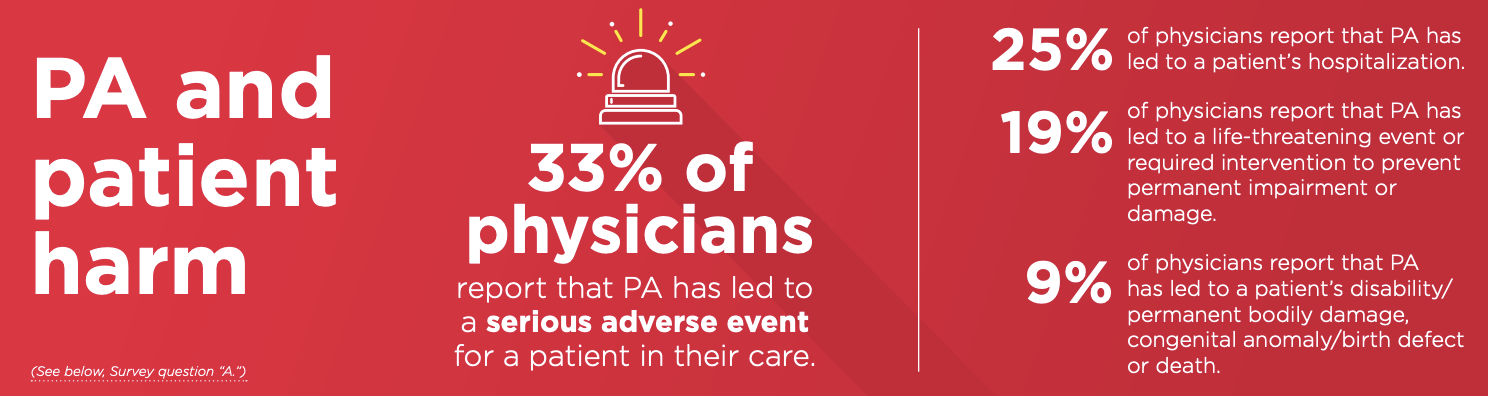


It's almost as though a conflict of interest exist between patients health and profit motive.
OH! PA means "Prior Authorization" and not "Physician's Assistant". Hell, the medical industry is just as bad or worse than the military when it comes to acronyms!
The amount of times I've heard medical folk say "Because of insurance we have to…." is entirely too many times. Insurance should support physicians and patients, NOT THE OTHER WAY AROUND!
I'm glad to see this is getting some attention.
I’ve often wondered why insurance companies are permitted to gainsay a doctor who decides a drug or treatment is necessary. The company hasn’t spoken to or examined the patient. Why isn’t this considered practicing medicine without a license?